

KEYWORDS
Conservative oxygenation, intensive care unit, mechanical ventilation, oxygen therapy, questionnaire, survey
INTRODUCTION
Optimal oxygen therapy in critical care remains a subject of debate. Almost all critically ill patients receive supplemental oxygen to prevent tissue hypoxia, but the appropriate oxygen dose remains unclear.1 Recent guidelines recommend targeting an oxygen saturation of 94-98% and stopping oxygen therapy when saturation reaches 96%.2,3 This recommendation is mainly based on observational studies suggesting harmful effects of liberal oxygen therapy.4-8 The first randomised controlled trial performed in one Italian ICU found an absolute mortality reduction of 8.6% for critically ill patients when limiting oxygen supplementation titrated to conservative oxygen saturation targets.9 However, a recent large multicentre randomised controlled trial found no difference in outcomes of adults undergoing conservative or usual oxygen therapy in the ICU, even though targeted oxygenation was frequently not achieved.10 In recent years, self-reported views of nurses and physicians with regards to oxygen therapy in critically ill patients have evolved towards a more restrictive approach. In the Netherlands, oxygen-induced lung injury was seen as a major concern.11 However, in actual clinical practice, these concerns were not accommodated, and the majority of partial pressure of oxygen (PaO2) values recorded were higher than self-reported targets. Hereafter, conservative oxygenation targets were introduced into daily clinical practice.5 A recent study showed an increase in the number of ICU clinicians concerned about oxygen-induced lung injury, which was also reflected in actual clinical practice.12 However, these Dutch studies were performed in three ICUs actively involved in research focused on oxygen therapy for critically ill patients. It therefore remains unknown whether these beliefs are widely supported and whether the results of previous studies can be generalised to ICU clinicians across the Netherlands. In the present study, we aimed to describe self-reported attitudes towards oxygen therapy from a large sample of ICU clinicians across the Netherlands. We further aimed to assess if there were differences in attitudes between nurses and physicians, age categories, and type of ICU.
MATERIALS AND METHODS
Questionnaire
The questionnaire was a translated and comprehensive version of previously used surveys from Canada and Australia/New Zealand, and was also previously used in the Netherlands.11-14 The anonymous online questionnaire consisted of 59 multiple-choice questions that were designed to elicit self-reported behaviour of ICU clinicians with respect to oxygen therapy in general and in specific case scenarios (complete questionnaire in Dutch: Supplement 1)*. It included questions about oxygen-induced lung injury, risks of mechanical ventilation, indices of tissue oxygenation, and arterial saturation (SaO2) and PaO2 targets for short and long-time periods in an acute respiratory distress syndrome (ARDS) patient receiving mechanical ventilation. The last part of the questionnaire investigated whether the respondent would adjust a fraction of inspired oxygen (FiO2) of 50% for given SaO2 and for given PaO2 in the following case scenarios: ARDS, cardiac ischaemia, cerebral ischaemia, sepsis, percutaneous coronary intervention (PCI) stent, and untreatable anaemia.
Target population
In April 2019, 36 ICUs in the Netherlands were approached with the request to send out a web-based questionnaire (LimeSurvey) to their nursing and medical staff. Subsequently, ICU clinicians were invited by email to complete the questionnaire. A reminder was sent out if deemed necessary. The invited ICUs included mixed medical and surgical adult ICUs in university and non-university hospitals across the Netherlands. The ethical reviewing board was informed and had no objection (G18.110).
Statistical analysis
Questionnaire responses are presented as a proportion of respondents per question. Differences in questionnaire responses between nurses and physicians, university and non-university ICUs and age categories were analysed using the Chi square test of Fisher’s exact test as appropriate. A p-value below 0.05 was considered statistically significant. Statistical analyses were conducted using R i386 3.4.4.
RESULTS
Characteristics of questionnaire respondents
Between April and August 2019, 1361 questionnaire responses were received from ICU clinicians (61% completed all questions). ICU clinicians from 28 (78%) out of 36 invited ICUs in the Netherlands participated in the online questionnaire. These 28 participating ICUs comprised the majority of all available ICU beds in the Netherlands (428 of 831 beds, data from the 2018 Dutch National Intensive Care Evaluation, https://stichting-nice. nl/datainbeeld/public). Two hundred-twenty-six (19%) ICU clinicians that participated in the questionnaire were from four university hospitals. Respondents consisted of 847 (71%) nurses, 287 (24%) physicians (8% residents, 1% fellows and 15% intensivists), and 53 (5%) with another type of practice (e.g., ventilation practitioner, physician’s assistant). Of the respondents, 258 (22%) were 18-30 years of age, 374 (32%) 31-40 years of age, 239 (20%) 41-50 years of age, 259 (22%) was 51-60 years of age, and 55 (5%) 61-70 years of age.
Questionnaire responses
The responses to questions regarding concerns when placing a patient on mechanical ventilation are listed in table 1. A majority (64%) of respondents considered oxygen-induced lung injury a major concern when initiating mechanical ventilation; 17% of respondents reported that high FiO2 posed a greater threat of lung injury than high tidal volumes and high ventilator pressures. Significantly more ICU nurses than physicians considered oxygen-induced lung injury a major concern during mechanical ventilation; 20% of the nurses reported that high FiO2 posed a greater threat of lung injury than high tidal volumes and high ventilator pressures, compared with 7% of physicians (p < 0.01). Compared to nurses, significantly fewer physicians would be concerned with a stable SaO2 of 85% within two hours (61% physicians vs. 81% nurses, p < 0.01). More clinicians from university ICUs responded that high tidal volumes and high ventilator pressures posed a greater threat of lung injury compared to clinicians from non-university ICUs (p = 0.01). Compared to university ICU clinicians, more clinicians from non-university ICUs reported they would begin to raise concern after a shorter duration of time with a stable SaO2 of 85% (p < 0.01). ICU clinicians of younger than 40 years of age more often reported they were majorly concerned with oxygen induced lung injury compared to older clinicians (p = 0.03).
Figure 1 shows the percentage of respondents accepting various oxygenation ranges in a young to middle-aged mechanically ventilated patient with ARDS. More physicians reported that lower SaO2 and PaO2 were acceptable, compared to nurses (supplementary table 1*, p < 0.01). More university ICU clinicians chose lower SaO2 ranges as lowest acceptable for under 15 minutes and 24-48 hours, compared to non-university clinicians (p < 0.01). Older ICU clinicians reported lower PaO2 as acceptable for up to 15 minutes (p = 0.01), compared to younger clinicians. 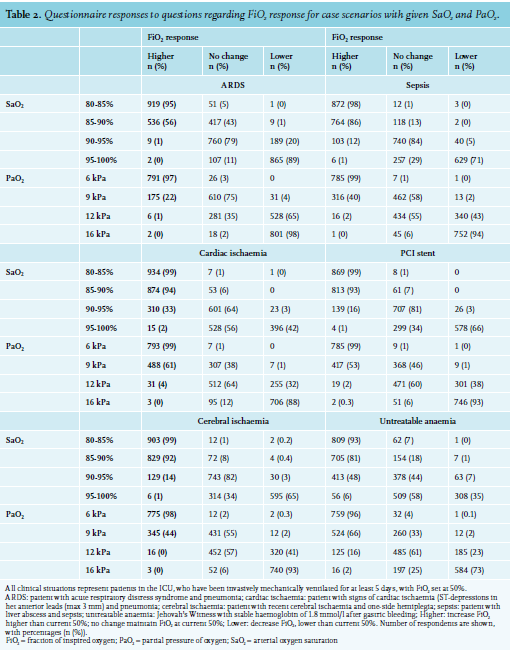
DISCUSSION
This national questionnaire study assessed clinicians working in the majority of ICUs across the Netherlands and showed that ICU clinicians consider oxygen-induced lung injury a major concern; high ventilator pressures and high tidal volumes were considered a greater threat than high FiO2. For shorter periods of time, ICU clinicians accepted SaO2 levels as low as 85% and PaO2 levels as low as 6 kPa (45 mmHg), but a higher limit of 90% and 7 kPa (53 mmHg) is preferred if the situation lasts longer. It seems that ICU clinicians consider a PaO2 of 6 kPa (45 mmHg) as too low, a PaO2 of 16 kPa (120 mmHg) as too high, and a PaO2 of 12 kPa (90 mmHg) as optimal, because they reported adjusting ventilation settings accordingly. In general, compared to nurses, physicians had a more open attitude towards conservative oxygen therapy and would allow lower SaO2 and PaO2 levels without adjusting FiO2. Older and university ICU clinicians would accept lower oxygenation, possibly due to more experience or more awareness of the potential adverse effects.
To our knowledge, this is the first nation-wide study describing self-reported attitudes towards oxygen therapy of ICU clinicians working in the 28 ICUs consisting of the majority of available beds and admissions in the Netherlands. Previous studies have focused on a selection of ICUs nationally or internationally.11,13,15,16 Perhaps, these ICUs were more oxygen-focused and this could have influenced the questionnaire results. We believe our results are a better reflection of the general attitudes of ICU clinicians towards oxygen therapy in daily critical care. The first study assessing attitudes of intensivists was performed in Canada in 1999 and found that 51% of respondents considered oxygen-induced lung injury a major concern.14 In our cohort of ICU clinicians, 64% reported oxygen-induced lung injury to be important, which was similar to results of a survey in 2013 of 90 ICU nurses and physicians in Australia.15 However, in 2010, 542 critical care nurses from Australia and New Zealand were surveyed and only 22% considered oxygen-induced lung injury a major concern.16 In our cohort, nearly 70% of ICU nurses considered it a significant concern. Apparently, the number of clinicians considering oxygen-induced lung injury in daily practice has increased over the years. This is most likely due to increasing evidence about oxygen-induced lung injury and the effect of conservative oxygen therapy on patient outcomes. However, apart from a time-dependent effect, it may also reflect a geographical difference or difference by chance. In a recent Dutch questionnaire study, performed after the implementation of a conservative oxygenation protocol in three ICUs, 76% of respondents considered oxygen-induced lung injury to be a major concern12, which was an increase of nearly 20% compared to the assessment before the implementation,11 and 10% more than what we found in this study. This supports our hypothesis that in ICUs where oxygen-related research is conducted clinicians are more concerned about oxygen-induced lung injury than in other ICUs.
Seventeen percent of the current respondents considered high FiO2 to be a greater threat of lung injury than high tidal volumes and ventilator pressures, which was similar to 13% previously found.13,14 This is remarkable, as evidence for lung-injury by high tidal volumes is well accepted,17 while evidence for the risks of high FiO2 in ICU patients is still controversial.9,10 Compared to an earlier study,16 we found that fewer nurses considered barotrauma to be a greater threat than high FiO2, compared to physicians. Possibly, physicians may be more often convinced by evidence of ventilator-induced lung injury due to high tidal volumes and pressures.18-20
The preferred PaO2 ranges for short and long time periods in an ARDS patient reported by the current respondents were comparable to the PaO2 range previously recommended in studies in ARDS patients by the ARDS Clinical Trials Network.21 These findings were similar to an earlier survey performed in critical care physicians from seven northern European countries where the majority chose a PaO2 of 10 kPa (75 mmHg) for an ARDS patient.22 Our questionnaire results also suggest that physicians tolerate lower PaO2 and SaO2 values than nurses. Physicians may be more comfortable with lower oxygenation and with taking actions and accountability with the risk of hypoxia. Physicians may also be better informed about the potential downsides of supplemental oxygen therapy. In a previous survey of nurses, more experienced nurses were more likely to answer that they would never be concerned with a stable SpO2 of 90%.16
Our study has the following clinical implications. As this study reflects the beliefs and attitudes of a representative sample of ICU clinicians from the Netherlands, the results may be useful to customise training, clinical decision making, and protocols. Furthermore, our study provides data for determining PaO2 and SaO2 targets in future interventional or observational studies. The current study also gives insight into the differences in attitudes of clinicians. These differences in attitudes could be explained by variances in education and training and by barriers experienced by the clinicians. When implementing new oxygenation strategies in daily critical care, it is important to acknowledge these differences of attitudes and actively engage and educate all clinicians to improve team compliance.
The primary strength of our study is its size and thereby its representativeness. The participation rate of 78% of the invited ICUs was high. In addition, participating ICUs consisted of more than half of the available ICU beds and more than half of all ICU admissions in the Netherlands in 2018. Moreover, the distribution of nurses and physicians was representative of a typical staff constitution of ICUs in the Netherlands. The questionnaire strongly resembles questionnaires previously used in other studies, allowing for comparisons and exploring trends over time and continents.11,13,14 Furthermore, our results show what clinicians think about oxygen therapy in critical care and for specific pathologies, which could be helpful when reviewing the impact of guidelines for critical care or specific pathologies. Our study has some limitations. The questionnaire data is self-reported and may not reflect actual practice and does not reflect the practice of non-responders. It has been shown that self-reported attitudes towards oxygen therapy are generally more conservative than actual practice.11 The cases included in the survey do not represent the complexity of patients in daily practice. SaO2 and PaO2 ranges and values in the survey were chosen arbitrarily. Because this was an explorative study, we chose not to correct for multiple testing.
In conclusion, our study provides new insights into the attitudes of ICU clinicians towards oxygen therapy across the Netherlands. The majority of ICU clinicians reported concern about oxygen-induced lung injury and preferred PaO2 and SaO2 targets in the lower physiological range. Physicians reported being more conservative with oxygen therapy and decreased FiO2 at lower SaO2 and PaO2 values, compared to nurses.
DISCLOSURES
All authors declare no conflicts of interest. No funding or financial support was received.
*The supplementary information (Dutch questionnaire / S-tables 1-4) is available upon request; please contact the corresponding author.
REFERENCES