

KEY WORDS
Hepatitis, listeria monocytogenes, listeriosis, liver abcesses
INTRODUCTION
Listeria monocytogenes are Gram-positive bacteria that are abundantly present in the environment. Contamination of fish, meat, vegetables, and dairy products can cause potentially fatal infections. Healthy individuals who are infected with Listeria may develop febrile gastroenteritis which usually lasts for one or two days and in this case, is self-limiting.1 However, in individuals of extreme age (neonates or elderly people) or in immunocompromised adults or pregnant women, listeriosis can be invasive, causing sepsis, meningoencephalitis, or infection of the pregnant uterus.1
In the Netherlands, listeriosis has been a compulsory notifiable disease since 2008. In 2017, 115 patients with listeriosis were registered.2 The most frequently registered manifestations were sepsis (37 patients), meningitis (27 patients), pneumonia, and gastroenteritis. In total, 10 patients (9%) died. The majority of patients in which listeriosis occurred were immunocompromised due to underlying disease or (immunosuppressive) medications. Possible sources of infection included soft cheeses, sausages, raw and boiled hams, chicken, and fish (e.g., smoked herring, a Dutch delicacy).
Even though liver involvement has been rarely described, it can, according to Scholing et al., manifest as solitary liver abscess, multiple liver abscesses, and diffuse or granulomatous hepatitis.3 In cases of listeriosis with multiple liver abscesses, the clinical outcome shows increased morbidity and mortality compared to presentations in which the liver is not involved.4 In this case report, we discuss an adult patient with listeriosis and liver involvement, who experienced a good clinical outcome.
CASE REPORT
A 73-year-old female presented to our Emergency Department with signs of sepsis. Her medical history showed hypertension and type 2 diabetes, for which she took metformin. At presentation, she had been sick for four days with a fever, headache, and drowsiness. At clinical examination, we saw a female who was visibly unwell. Her blood pressure was 120/80 mmHg with a tachycardia of 100-120 beats per minute, her rectal temperature was 39.9°C, and respiratory rate was 20 breaths per minute. The remaining physical examination revealed no other potential diagnostic clues and she did not present signs of meningitis. The laboratory results (table 1) showed increased inflammation parameters with electrolyte disturbances and kidney dysfunction most likely due to sepsis.
The patient’s laboratory tests showed elevated liver enzymes and prolonged time of coagulation tests. A chest X-ray and urinary sediment were normal. A computed tomography (CT) scan of her thorax / abdomen showed a liver with multiple small round lesions with a density of 30-40 Hounsfield units and circular colouring, at first, appearing to be malignant metastases (figure 2). 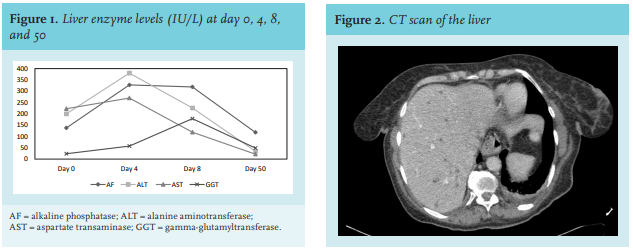
However, the scan showed no observable lymphadenopathy or any primary (malignant) tumour. The patient was admitted to the Internal Medicine ward and empirical treatment for sepsis was started, consisting of 1000/200 mg amoxicillin/clavulanate, four times a day and gentamicin 4 mg/kg, once a day, intravenously (i.v.) according to local guidelines.
Clinically, the patient recovered after two days of antibiotics. Kidney function and electrolytes were restored after fluid administration. However, liver enzymes increased with a peak level at day four (figure 1). Ultrasound investigation of the liver showed the same round lesions as seen on the CT scan with a largest diameter of 1.2 cm. Unfortunately, the lesions were too small or not well located, and we were unable to perform needle aspiration. One of two blood culture bottles (BD BACTEC) taken on admission showed growth of an apparently anaerobic Gram-negative rod after two days of incubation. However, overnight culture on solid media revealed a Gram-positive rod. This was subsequently identified as Listeria monocytogenes with matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI TOF MS; bioMerieux, Marcy-l’Etoile, France). The antibiotic therapy was changed into i.v. amoxicillin 1000 mg, six times a day and continued for a total period of three weeks. Most liver tests improved after four days of antibiotic therapy. A second CT scan of the liver at day 15 of admission (day 19 after the onset of symptoms) showed a significant reduction in the amount and size of the lesions. The patient was discharged from our hospital after 22 days, in excellent clinical condition. Follow up at day 50 showed almost normalised laboratory results and on CT scan, a completely normal liver without any lesions.
DISCUSSION
In this case, hepatic inflammation and dysfunction was secondary to disseminated listeriosis. This was indicated by the marked improvement of liver enzymes and decrease in amount and size of the liver lesions in response to antibiotic treatment. Liver involvement in listeriosis is rarely reported in the literature, which is surprising, considering the important role attributed to the portal vein system in the pathogenesis of invasive L. monocytogenes disease.5
In a systematic literature review published in 2007, Scholing et al. compared 34 cases of Listeria infection with liver involvement. In 13 cases (38%), the underlying condition was type 2 diabetes, as was the case in our patient. Our case, however, differed with respect to two key characteristics: mode of liver presentation and the outcome. Scholing et al. reported on 10 patients, each with a solitary liver abscess; 11 patients with multiple small liver abscesses; and 14 patients with diffuse (10) or granulomatous (4) hepatitis (as diagnosed by clinical presentation, biopsy, or autopsy). Interestingly, liver enzymes (alanine transaminase and aspartate aminotransferase) were grossly elevated in all patients who suffered from diffuse hepatitis, but such elevation, in general, was not a good predictor of solitary or multiple liver abscesses. Furthermore, all patients with a solitary abscess had excellent clinical outcome after drainage of the abscesses and antibiotic treatment. In the 11 patients with multiple liver abscesses, three patients were treated with abscess drainage and survived; the other patients died. However, in the 10 patients with diffuse hepatitis, the survival rate was 70%, with systemic antibiotic administration for a mean treatment period of three weeks. In our patient, we observed radiological signs of multiple small liver abscesses together with a 10-fold liver enzyme elevation. The latter could have been the direct result of the multiple abscesses, although an alternative explanation may indicate the presence of concomitant hepatitis. Elevated liver enzymes were observed in only 4 of 21 patients with solitary or multiple abscesses described in the review; however, diagnosis made by biopsy or autopsy was performed in only six of the 10 patients with laboratory tests suggesting diffuse hepatitis. In the other cases, the diagnosis ‘hepatitis’ was made based on clinical presentation, which included a 7-160-fold liver enzyme increase. Therefore, it is uncertain if these patients had underlying liver abscesses.
In a short review of diffuse hepatitis in listeriosis, Yu et al. described a case with clinical and laboratory findings of diffuse hepatitis, but postmortem examination revealed that the liver parenchyma was studded with firm yellowish nodules, which turned out to be miliary abscesses.6 Ultrasound of the liver from our patient during the first week after admission showed an inhomogeneous liver with a large amount of strongly echogenic, small, round lesions, which were scattered throughout the parenchyma in a patchy pattern. Although they seemed to be metastases, as observed by CT scan, by ultrasound they appeared to be miliary abscesses because of the echo density and a sharply defined back wall. The noncancerous nature of these liver abnormalities was confirmed by the fact that after treatment with antibiotics, the liver tests had normalised, and all liver lesions had disappeared. We hypothesise that this might reflect a similar manifestation of miliary abscesses with concomitant necrosis with or without hepatitis, which could explain the observed liver enzyme elevation.
Fortunately, our patient had an excellent clinical outcome after three weeks of intravenous antibiotics, despite our inability to perform drainage of the abscesses. This is in contrast to previous literature. One reason could be the relatively quick administration of antibiotics, which was started four days after the onset of symptoms. Also, amoxicillin-clavulanate, together with gentamycin, is the first choice of treatment in sepsis of unknown origin in our local guidelines, so our patient received adequate antibiotic therapy immediately after hospital presentation. In many Dutch hospitals, sepsis with unknown cause is initially treated with cephalosporins, which in this case, would have delayed effective treatment up to the moment the Listeria was diagnosed.
CONCLUSION
In this case report, we show that small liver abscesses caused by a Listeria monocytogenes infection can clinically mimic hepatitis, as suggested by the elevated liver enzymes. Therefore, the classification of possible liver involvement in listeriosis (a solitary abscess, multiple abscesses, or hepatitis) contains clinical conditions that are not mutually exclusive. In addition, it may be of value to add an additional classification category, for example, hepatitis mimicry due to miliary liver abscesses. It is important to keep in mind that multiple liver abscesses do not necessarily yield a poor prognosis, even in the absence of drainage. Further research is needed to identify the mechanisms of liver involvement in listeriosis and which factors affect prognosis.
DISCLOSURES
All authors declare no conflicts of interest. No funding or financial support was received.
REFERENCES