

KEYWORDS
Intensive care, invasive procedures, non-physician provider, nurse practitioner, physician assistant, cost-effectiveness
INTRODUCTION
Both the scale at which nurse practitioners (NP) and physician assistants (PA) are implemented and their exact tasks and responsibilities on the intensive care units (ICUs) throughout Europe remain unclear. Nevertheless, these non-physician providers are already employed with equal competences to residents in some ICUs in European countries. Although implemented in ICU staff, European literature on this subject is lacking, with the only research being conducted in the United States of America (USA).
Available research from the USA shows that from 1960 until the 1990s the NP as well as the PA were implemented in the ICU. Back then, they were mainly introduced in regions with physician shortage to execute the tasks normally done by resident physicians. Their role was based on a natural evolvement from registered nurse in the ICU to an acute care nurse practitioner (ACNP) who could provide the necessary medical care for patients. Because the ACNP became indispensable on several American ICUs and emergency departments, the ACNP received a legislated title in the 1990s.
In 2008 the review by Kleinpell et al. concluded that ACNPs and PAs on the ICU provided high-quality care which was non-inferior to that of residents.1 The ICU length of stay (LOS) and mortality were comparable if patients were treated by teams with ACNPs and an intensivist or by teams consisting of residents or fellows and an intensivist. In contrast to the non-inferiority, the advantage of ACNPs was their continuity of care and an experienced ACNP needed less supervision from intensivists compared with residents doing an internship. Moreover, a review of 2012 by Edkins et al. revealed that ACNPs provided high-quality care at a low cost.2
Around the year 2000, the general concept of NPs and PAs in medicine and their training course was also recognised in the Netherlands because of an expected increase in healthcare demand as a result of economic welfare and the ageing population.3 They were also implemented in some ICUs. Although the function of NPs and PAs on the ICU is similar to the tasks performed by ACNPs, ACNPs mostly cover a broader part of acute care and their comparable legislated title has not yet been introduced in the Netherlands. The theoretical and practical skills of the NPs and PAs on the ICU, however, are comparable with those of ACNPs and similar to the job description of residents on the ICU. Therefore, the more generally accepted term ‘acute non-physician providers (NPP)’ will be used in this article to refer to NPs and PAs working on the ICU.
The aim of this paper is to describe the course of training and implementation of an alternative ICU staffing model with NPPs besides residents and intensivists in the Netherlands. In addition, a description of the invasive procedures performed by NPPs, residents or intensivists is reported with a retrospective cohort analysis to provide some insights on the quality of care and one of the tasks of NPPs on a high volume ICU in the Netherlands.
METHODS
Setting
Catharina Hospital is a tertiary hospital in Eindhoven, the Netherlands containing all medical specialties, except for complex neurosurgical patients who require intensive care admission. The hospital has a 33-bed mixed medical and surgical ICU and provides care as a referral centre for the region with the characteristics described in table 1. The medical staff of the ICU consists of intensivists, 8.8 fulltime-equivalent (FTE), supported by residents, residents in training and NPPs for which the FTEs are reported in table 2. Residents in training are on a rotating schedule of 3 to 4 months in which ICU experience is mandatory for their specialist training. The weekly required hours for residents, residents in training and NPPs are equal and 38 hours per week according to a local agreement.
The nurse practitioner training course
For ten years now, the training program to obtain a master degree of acute care nurse practitioner (NP) is available in Catharina Hospital together with Fontys University of Applied Sciences. A minimum of four years’ experience as an ICU nurse was arbitrarily chosen as a local requirement to be eligible for the acute care NP training as a certain settlement in and acknowledgement from the nursing group is required to attain the supervising role of an acute care NP. In 2016 the NP training consisted of theoretical medical skills, practical skills and nursing skills. For the theoretical medical skills, participants are trained in clinical reasoning based on broad medical and pathophysiological insights to create differential diagnoses. The nursing part includes training in nursing diagnosis, such as recognising problems like fear, discomfort and decubitus combined with the aim to prevent these problems. The practical part consists of two years of hands-on clinical physician work on the ICU, like the resident physicians, with the focus on the different medical specialties and their problems. After graduation, the acute care NP has the same job description and responsibilities as the resident.
The physician assistant training course
In contrast to the NP training course, the physician assistant (PA) training course is more focused on the medical domain and consists of a theoretical part, which attends to medical problems in all specialties from psychiatry, surgery to internal medicine. The participants are assessed with multiple station exams in which the participant has to solve clinical problems, propose therapies and prescribe medication. The practical part consists of hands-on training on the ICU and traineeships within several specialties. Graduation also results in a master degree with the same job description as the residents in the ICU. This course is also provided in Catharina Hospital together with HAN University of Applied Sciences.
Job description
Both the NP and the PA master degrees grant permission to legally perform medical care on the ICU, such as making treatment plans including prescribing treatment medication, presenting at multidisciplinary meetings, and performing invasive procedures. A specialist always supervises these tasks, which in this case is an intensivist. There is no difference in practice between the NPs and PAs on the ICU. Both have the same competences and tasks as all residents on the ICU. These NPPs perform some extra tasks such as improving local ICU protocols and, like intensivists, they are also involved in guiding new residents, as mentors, during their first month on the ICU to familiarise them with the ICU and protocols.
In Catharina Hospital, the day shift of NPPs is made up of various components, which start with a morning handover. After this collective handover the NPPs and residents start off with the clinical examination of the admitted ICU patients. Both NPPs and residents compose an initial treatment plan with optional additional examinations based on their findings. This proposed plan is assessed and adjusted, if necessary, by the intensivist during the ward round at the end of the morning. In the beginning of the afternoon the NPPs and residents report the main problems with the initiated treatment of all admitted patients in a multidisciplinary meeting containing representatives of all relevant specialties and three intensivists. After this meeting the NPPs and residents take care of the additional requested examinations, check all prescribed medication and communicate with family. If necessary, the NPPs or residents can perform invasive procedures, such as insertion of central venous or arterial lines, thoracotomies with tube insertion, intubations and electro-cardioversion. Only arterial lines or peripheral venous catheters are placed without supervision of the intensivist if the NPP or resident who is taking care of the patient is confident enough. If not confident or in case of one of the other interventions, the intensivist decides whether the invasive procedure needs to be supervised based on the characteristics of the patient and the NPPs’ or residents’ experience and his or her confidence. Supervision ranges from observation to hands-on guidance. All upper central venous accesses are performed by either the intensivist or NPP since residents have limited experience in placing upper central venous catheters. Ultrasound for additional guidance is used when deemed necessary. The day shift ends after eight hours with a handover. Two NPPs, two residents, or one NPP and one resident cover the eight-hour shifts of the evening and night. Those in attendance are responsible for all admitted ICU patients, resolve problems that may emerge and can perform invasive procedures. Besides these duties during these shifts, both NPPs and residents are part of the rapid response team in Catharina Hospital. 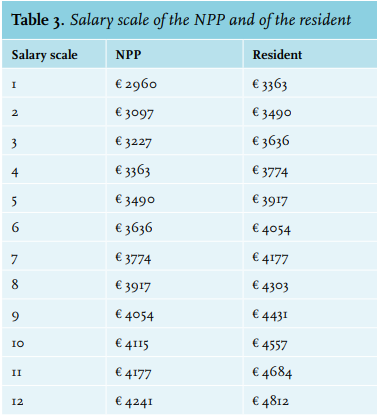
Since 2015, all patients undergoing an invasive procedure by an NPP are entered in the quality database of NPPs. The data of 2015 and 2016 were extracted and loaded into Microsoft Excel 2013 in an anonymised manner. Since 2016 the inserted central venous or arterial catheters on the ICU, which are entered in a central hospital database to monitor the number the catheter-related bloodstream infections, could be attributed to either residents together with intensivists or NPPs. All these databases are prospective databases with variables such as medical history, relevant medical scoring systems, the diagnosis, complications and interventions. After extracting these data and comparing them with the separate NPPs’ quality database, the study group was able to recognise which catheters were inserted by the group of NPPs or inserted by the group of residents and intensivists, or by intensivists in case of upper central venous lines during 2016. It was only possible to determine if a catheter was inserted with or without the supervision of an intensivist for catheters inserted by the NPPs. For the group of residents and intensivists it was not possible to determine whether a venous or arterial catheter was inserted by either the intensivist or the resident, or by the residents with supervision of the intensivist. However, arterial catheters are mostly inserted without supervision by either NPPs or residents and not by intensivists. The number of inserted catheters was plotted against the fulltime-equivalent (FTE). An ultrasound was available for guidance and its use depended on the preference of the person placing the line combined with patient characteristics.
Because of the descriptive nature of this study we collected a diverse amount of outcomes of interest. First of all the baseline characteristics of the ICU in 2015 and 2016 were collected to give an overview of the general ICU performance and the ICU population. The collected baseline characteristics were age, Simplified Acute Physiology Score (SAPS II), ICU and hospital mortality, standardised mortality ratio correct for the APACHE IV score and the SAPS II, and the length of stay on the ICU and in the hospital. Second, the number and device characteristics of documented invasive procedures combined with the number of procedural complications for central venous catheter (CVC) insertions were recorded. The included invasive procedures were insertion of central venous or arterial catheters, thoracotomies with tube insertion, intubations and electro-cardioversion. Procedural complications were pneumothorax, recognised on chest radiograph; major bleeding, defined as bleeding causing haemodynamic instability or endangering vascularisation of the limbs; catheter-related bloodstream infections (CLABSI), defined as a primary bloodstream infection in a patient who had a central catheter inserted within the 48-hour period before the developing the infection and that is not bloodstream related to an infection at another site;4 and malposition based on the upper CVC defined as tip placement in the distal portion of the superior vena cava just above the junction with the right atrium (cardiac silhouette) as judged by a radiologist.
To gain insight into the costs of NPPs and residents, the salary scales of both were adapted from the collective hospital labour agreement of the Dutch Hospital Association (table 3). The FTE for residents, residents in training, and NPPs on the ICU in Catharina Hospital was equal and consists of 38 hours a week.
Statistical analysis
Statistical analysis was performed with Microsoft Excel 2013. The data for this retrospective cohort study are described as numbers or percentages or given as a mean with standard deviation. A median and interquartile range are shown if the data were not normally distributed.
RESULTS
The baseline characteristics of all admitted ICU patients in 2015 and 2016 are summarised in table 1. The number of admissions, mean age, SAPS II, standardised mortality ratios and length of stay were alike for both years.
In 2015 and 2016, NPPs performed 251 and 407 invasive procedures, which were 58.6 and 113.1 procedures per FTE, respectively. Figure 1 shows the distribution of all invasive procedures that were performed by the NPPs for 2015 and 2016. Figure 2 demonstrates the distribution for which CVCs and which arterial catheters were performed by unsupervised NPPs, by residents supervised by NPPs, by NPPs supervised by intensivists, and by residents or intensivists in 2016. The total number of CVCs inserted by NPPs and physicians together in 2016 was 125. Of these CVCs, 58% (n = 73) were inserted by or under supervision of NPPs, while 42% (n = 52) were inserted by residents or intensivists or by an NPP supervised by an intensivist (figure 2). The incidence of CVC insertions by NPPs was 20 per FTE, while the incidence of CVC insertion by residents, with or without supervision, was 4.3 per FTE and 2.5 per FTE if the 8.8 FTEs of the intensivists were taken into account along with the residents.
The incidence of inserting arterial catheters combined with supervising arterial cannulation all by NPPs was 61.7 per FTE and if the rest of the arterial catheter insertions were distributed over only residents the incidence was 11.8 per FTE. When both the FTEs of intensivists and residents are taken into account, this incidence becomes 6.9 per FTE. Both the number of intubations and thoracotomies by NPPs increased in 2016 compared with 2015. The increased number of thoracotomies was explained by the fact that most NPPs became self-dependent in performing this procedure. In 2015 only the complication rate of CVCs inserted by NPPs was available; there were two misplacements and one failure to place. Of all invasive procedures with CVCs, there were five complications for NPPs and intensivists together in 2016, all while placing upper CVCs. There was one pneumothorax caused by an NPP during insertion of a subclavian catheter. There was one CLABSI 14 days after insertion of a CVC by an NPP. Three complications arose during attempts to insert a CVC by an intensivist in one single patient. There was a pneumothorax and mediastinal bleeding after an attempt of placement of a subclavian catheter. After this attempt an ultrasound guided jugular catheter was inserted too deep (in the right atrium). The data over 2015 and 2016 for NPPs showed two misplacements, one failure to place and one pneumothorax. There were no other complications during the invasive procedures documented.
The salary scale of NPPs and residents is depicted in table 3. The payment in Euros represents the salary per month. The increments of salary are represented by the numbers in the first column and increase once per working year.
DISCUSSION
This descriptive study shows how intensive care nurses can be successfully trained locally, based on a university program, and be implemented as NPPs on the ICU. The included retrospective cohort analysis demonstrates that NPPs perform more invasive line insertions per FTE than intensivists or residents, with a complication rate that is up to standard and comparable with that of the intensivist. These findings show that implementation of NPPs can result in a reduction in the workload of intensivists who can then allocate time to other tasks. In addition, both the NPPs’ experience and thorough knowledge of the ICU may add a quality impulse to ICU care.
Although the results of this descriptive study may indicate a beneficial role for NPPs on the ICU, the concept of an NPP in the Netherlands and Europe remains relatively unknown. There is no Dutch or European medical evidence available describing the role and potential advantages of NPPs on the ICU. This lack of literature is becoming increasingly important; such evidence may even be essential, since ICU medicine and therefore ICUs are undergoing change. Nowadays, Dutch intensivists mainly work in a closed format which means that they have the final responsibility for their ICU patients and their daily treatment plans. They base their treatment on their own knowledge combined with the advice requested from other specialists. Compared with the earlier days of the ICU, where the surgeon, internist or other specialists treated the patient on the ICU, this change has improved the quality of care, but also intensified the workload on the ICU. NPPs may be a viable staffing alternative to achieve the goal of managing increasing workloads while retaining a high quality of care.
In the foreseeable future more changes can be expected, such as a physician shortage due to advances in complex medical techniques, the increasing age of ICU patients and migration of physicians to cities.5,6 Some rural areas of Europe are already coping with physician shortage.7-9 Although there is not yet a shortage of intensivists in the Netherlands, finding nurses and residents to cover 24/7 shifts on the ICU is becoming more difficult due to duty hour restrictions of residents and the desire to work in specific areas of the country.
Moreover, the quality of care of residents on the ICU could be organised more efficiently. For most residents the ICU internship is their first encounter with ICU care. Their time for acquiring knowledge and experience in this area mostly remains limited due to their rotating internships for the specialist training. Training of these residents consumes time and the quality improvement of this training on ICU care only becomes noticeable at the end of their internship. Both reasons, the availability of residents and their limited experience, affect the continuity and quality of daily ICU care and may provide opportunities for the NPP.
Both residents and NPPs require training and supervision by intensivists. While the training to become an NPP takes longer, a reasonable assumption is that in the end residents require more training time and supervision as they consist of a larger group, generally have no ICU experience, and continuously rotate after a mean of 3-4 months resulting in limited time to profit from their acquired experience. In addition, since NPPs already worked on the ICU as nurses they know the local protocols and require less supervision from the intensivists. This knowledge even makes it possible for them to guide the new residents on the ICU by explaining local protocols and training or supervising the more simple interventions.
The second part of this descriptive study underscores a potential advantage of implementing NPPs by describing routine invasive procedures in the ICU. The number of inserted venous and arterial catheters per FTE was higher for NPPs (CVC: 20/FTE, arterial catheters 61.7/FTE) than for residents and intensivists together (CVC: 4.3/FTE, arterial catheters: 11.8/FTE). Although information bias could have influenced these numbers, the hypothesis could be that these numbers are due to NPPs not being subjected to time limited experience on the ICU, in contrast to the residents. This experience results in their capability to insert venous and arterial catheters without the supervision of an intensivist. Our observed complication rate of the NPP data from 2015 and 2016 was in line with the study by Alexandrou et al. Their comparable complication rate during a 13-year follow-up of a catheter insertion service executed by non-physicians of the ICU is up to the international standards.10-12 Moreover, figure 2 shows that NPPs are indeed able to educate and supervise residents in our hospital. These examples indicate that NPPs can facilitate a broader span of control of the intensivist by taking over some of the tasks with the same quality of care. A further advantage of this workflow is centralisation of these interventions, which is in line with the observed success and complication rate.
American literature already supports implementation of NPPs by reporting a quality impulse on several aspects of ICU care. Both mortality and length of stay on the ICU and in the hospital remain the same or are even slightly better in cohorts of ICUs with NPPs compared with ICUs staffed by only residents and intensivists.13-17 Additionally, one study analysed the communication between nurses, non-physicians and physicians and found a satisfactory communication of NPPs by all groups and a better communication of NPPs than physicians from the perspective of some groups.18
This is in line with the study by Rayo et al. which suggests better comprehended hand-overs and patient orders by experienced NPPs compared with new residents.19 These results refer to the problems residents encounter on the ICU in terms of understanding and carrying out orders during multidisciplinary meetings.20 Both outcomes can be explained by ICU-NPPs being more experienced in protocols, routine ICU processes and familiarity with patient orders on the ICU than most residents.
All these benefits can provide improved continuity of quality for care on ICUs, which is the primary reason for considering implementing NPPs. Whether this quality improvement by NPPs is also cost-effective remains an unanswered question. Although several studies address this question, it remains difficult to extrapolate their results to other ICUs, as the workflow in each ICU can differ significantly. However, one can hypothesise that outsourcing several tasks of an intensivist to a more inexpensive NPP can save intensivists time and be cost-effective. Based on the plain salaries, NPPs cost more than residents in the long term. The extra costs come with the potential benefit of quality improvement as a result of the NPPs’ continuity and experience on the ICU.
Limitations
The most important limitations are inherent to the retrospective cohort design of this study and description of one single ICU. The first limitation is selection bias as the more difficult invasive interventions are more likely to be done by the most experienced person available, so the NPP or the intensivist. This could explain the higher number of interventions performed by the NPPs compared with residents. It can also overestimate the number of complications caused by intensivists as they potentially had to insert upper CVCs in more sick or less technically accessible patients.
Considering the data collection, retrieving data on catheter insertions performed by residents or intensivists was only possible in the year 2016, while NPPs’ data could be obtained over the years 2015 and 2016. Moreover, the aggregated data of intensivists and residents made a desired in-depth comparison between residents and NPPs impossible. Additionally, the second bias is the information bias. This could underestimate the number of performed interventions of residents as in our experience they underreport interventions more often since they do not have a separate database. Co-intervention bias is a third possible bias as potentially one group could have increased the use of ultrasound in the analysed years.
Comparability between residents and NPPs remains difficult. In general, residents have less ICU experience than NPPs due to their shorter presence on the ICU. In contrast, this limited time and therefore experience are also one of the main reasons for considering implementation of NPPs. Their continuity, experience and knowledge of ICU processes is the main advantage. Finally, this study describes a training course and staffing model with NPPs in one single centre and therefore results can be different in other ICUs with other case mixes.
CONCLUSION
This descriptive report covers a successful local method of implementing NPPs on the ICU, as a new staffing model concept in Europe. To provide insight on the quality of their skills, an included retrospective cohort analysis indicates that the quality of invasive procedures with a low complication rate seems comparable between NPPs, and residents and intensivists. Whether sustainable quality improvement can be achieved with NPPs in the ICU setting should be subject to further study, both in the Netherlands and in Europe.
DISCLOSURES
All authors declare no conflict of interest. No funding or financial support was received.
REFERENCES