

KEYWORDS
Anabolic androgenic steroids, AAS, performance enhancing drugs, PED, hypogonadism, bodybuilding, illicit drug use
INTRODUCTION
AAS abuse in the Netherlands
In the Netherlands approximately 160,000 people use performance enhancing drugs (PED), of which 20,000 anabolic androgen steroids (AAS).1 Production and trading of AAS without a license is prohibited in the Netherlands, yet AAS can be easily acquired illegally through local dealers or the internet. The majority of users do not engage in organised sporting events.1
AAS is most often used intermittently, i.e. in cycles, and users’ knowledge is based on information from acquaintances, trainers or the internet.2 Among users, cycles differ greatly with respect to length, dosage as well as the number of different AAS used simultaneously or consecutively.3 An earlier report showed that in about 50% of illegally obtained AAS the contents do not match the description on the label.4 Therefore, it is difficult to attribute side effects to specific AAS or dosages.
Health concerns about AAS abuse
The Health Council of the Netherlands stated that AAS are harmful but data are lacking as to precisely how harmful they are.5 Among physicians, there is low awareness of the possibility of AAS abuse by patients, and patients tend to be secretive about their use and do not rely on the physician’s knowledge of AAS.6 Knowledge of the unwanted somatic and psychological effects of AAS is limited because clinical research in the field of AAS is scarce. Prospective clinical trials among AAS users are hampered by ethical issues due to the fact that there is no registered indication for the use of supraphysiological doses of androgens, the products are mainly illegally obtained and most anabolic steroids are not registered for, nor extensively studied in, humans. As a result, most knowledge about the harmful effects of AAS is based on low level evidence, such as expert opinion, case reports or small observational studies.
Outpatient AAS clinic
An outpatient clinic for past and current users of AAS, the ‘Anabolenpoli’ or AAS clinic, was established in the Spaarne Gasthuis, Haarlem in 2011, in an attempt to gain more insight into the characteristics of AAS users, the methods of AAS use and the health risks associated with AAS abuse in the Netherlands. To our knowledge, it is the only clinic worldwide that focuses primarily on helping patients with health problems related to AAS. Patients need a referral to the clinic from their general practitioner or a medical specialist and the healthcare provided is fully covered by Dutch healthcare insurance. Haarlem is located centrally in the Netherlands with a maximum distance of 250 km to all country borders and is therefore readily reached by patients throughout the country.
The AAS clinic has now been running for five years. This study provides an overview of all patients who were referred to the clinic and generates novel data regarding recreational AAS use in the Netherlands and related health issues.
MATERIALS AND METHODS
Consultation at the AAS clinic
During consultation of each patient at the AAS clinic, the history of AAS use was assessed. Items discussed were the reasons for referral, the age at which the patient used AAS for the first time, the number of cycles completed, the number of years of active AAS use (every year with at least one cycle), and whether a patient had used continuously (defined as AAS use without interruptions for at least one year). Additionally, the types of AAS that a patient had used were inquired about as well as the use of other PED, medications to prevent or treat side effects, some of which are referred to as post-cycle therapy (PCT), with corresponding dosages. Patients were routinely asked which side effects were experienced during AAS use. All patients had a routine medical check including history and physical examination. If indicated, additional investigations were done, such as blood tests, urinalysis, semen analysis or electrocardiography.
Review of cases
For this study, all case files were reviewed for reasons for referral, patient and demographic characteristics, history and methods of AAS use, reported side effects, and use of other PED or medications. An overview was made of the investigations performed by the referring physicians as well as those ordered by the clinic, conclusions drawn and diagnoses established, and therapies employed. If available, follow-up data were recorded.
Descriptive analysis
Simple descriptive statistics were used to display quantitative data. If the variables were normally distributed, mean and standard deviation were calculated. If the distribution of a variable was skewed, a median is presented with a range. Documentation of the variables analysed was not complete in all case files. Data were frequently missing, for example for employment status, drug use or side effects. Therefore, percentages displayed in the results section (and tables) are not the percentages of all 180 patients but rather the percentage of patients from whom the data could be retrieved (numbers are indicated if applicable).
RESULTS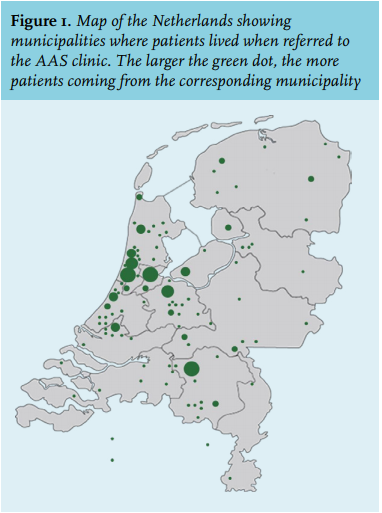
In total 180 patients visited the AAS clinic between May 2011 and May 2016. The number of patients referred annually was between 30 and 40. Patients came from municipalities throughout the Netherlands, and Belgium, as shown in figure 1. Patient characteristics are displayed in table 1. Patients had a mean age of 34 years (range 19-61) and 99% were male. The patients invariably engaged in physical strength sports, with 81% being former or current bodybuilders. Of the patients, 88% were not on AAS at the time of consultation. The reasons for referring a patient to the AAS clinic are presented in table 2 and were related to symptoms occurring during or after a cycle (48%), suspected hypogonadism (10%) or abnormal blood tests (7%).
METHODS OF USING AAS
Characteristics of AAS use by the patients and types of AAS used are summarised in table 3. The patients had a median age of 23 years (range 16-53) when they first used AAS. Of the patients, 94% used in cycles but 20% at some point used AAS uninterruptedly for more than 12 months. The number of cycles completed and the mean duration of a cycle per patient are shown in figure 2. Most visitors had completed more than three cycles prior to their visit. The duration of cycles varied considerably. However, most cycles lasted between 6 and 18 weeks. Cycles mostly consisted of two or more different anabolic steroids. Products were used simultaneously or consecutively, and the dose, duration and combination of the different products used in the cycle differed substantially between cycles. Injectable testosterone esters were used by 80% of users, mostly combined with nandrolone, trenbolone, stanozolol and/or boldenone.
OTHER PED, MEDICATIONS AND PCT
Other substances used in addition to AAS are shown in table 4. Growth hormone was the most popular PED followed by clenbuterol and thyroid hormone. Medications used during or shortly after a cycle of AAS were aromatase inhibitors (anastrozole, exemestane and letrozole), anti-oestrogens (clomiphene citrate or tamoxifen), human choriogonadotropin (hCG), isotretinoin, sildenafil, diuretics and finasteride. Of the patients, 94 (71%) always used PCT following AAS use for a mean period of four weeks, whereas 28 (21%) patients never used PCT. Agents used in PCT were mainly tamoxifen, hCG and clomiphene citrate.
REPORTED SIDE EFFECTS
Of the patients, 96% reported at least one side effect attributed to the use of AAS (table 5). Particularly common were acne, decreased libido, testicular atrophy and gynaecomastia. A general distinction could be made between side effects that occur during a cycle, i.e. gynaecomastia, fluid retention and aggressiveness, and those occurring after a cycle, i.e. erectile dysfunction and decreased libido. Of the reported health issues, none had led to hospital admission, except for a severe skin infection in one patient at an AAS injection site.
Additional investigations
If appropriate, additional tests were performed to investigate the relationship between reported health issues and AAS use. The results of blood tests, urinalysis and semen analysis are summarised in table 6. An elevated level of serum creatine kinase (CK) was observed in 45% of the tested patients. Of the six patients with a CK elevated 10 or more times the upper limit of the reference range, five were using or recently finished using AAS. The CK was restored to normal at repeat testing in the remaining patient. In one patient the liver biochemistry had been markedly abnormal during AAS use (7-8 times upper limit of ALAT reference range) but fully recovered when AAS were discontinued. An elevated plasma creatinine level (with a corresponding eGFR < 45 ml/min/1.73 m2 calculated by the MDRD formula) was observed in two patients, of whom one had a previously diagnosed IgA nephropathy and the other used creatine ethyl ester (CEE) supplements daily. CEE is known to increase the plasma creatinine level, unrelated to kidney function.7 After discontinuing the supplements, the creatinine level returned to normal. Polycythaemia (haematocrit > 55 %) occurred in four patients but was mild except for one patient who used a maintenance dose of Sustanon and required regular phlebotomy therapy.
Electrocardiography was performed in 24 patients and did not reveal any abnormalities except for one patient with positive voltage criteria for left ventricular hypertrophy. In one case, an MRI was performed to exclude a pituitary tumour as blood tests had revealed hyperprolactinaemia. In another case, karyotyping was used to demonstrate the Klinefelter syndrome as blood tests had showed hypergonadotropic hypogonadism which is not expected after current or previous AAS use. Furthermore, in one case hepatitis virus serology and liver ultrasound was performed to analyse abnormal liver biochemistry. No explanation was found but a relationship with AAS use was less likely as the liver enzymes remained elevated after discontinuation of AAS.
Diagnoses and treatment
Treatment of symptoms usually consisted of patient education, reassurance and advice. The general recommendation was not to use AAS again. Gynaecomastia was observed in 18 cases and treated with tamoxifen in eight but usually relapsed after discontinuation. In total six patients with gynaecomastia were referred to a plastic surgeon for extraction of breast tissue. Reduced fertility related to AAS use was diagnosed in five patients and treated temporarily with tamoxifen in two and hCG in one. There are no follow-up data to confirm whether treatment was effective in these patients except for the patient treated with hCG who did not recover. Azoospermia due to AAS was not seen. One case of infertility was explained as posttraumatic obstructive azoospermia. Temporary and long-term (> 1 year) post-AAS hypogonadism, defined as androgen deficiency due to AAS use, was established in 37 and 19 cases, respectively. Patients with long-term post-AAS hypogonadism had a significantly longer history of AAS use with a mean of 11 years compared with 6 years in the rest of the patient population (unpaired t-test, p = 0.001). In 17 patients with post-AAS hypogonadism, tamoxifen was prescribed temporarily to enhance endogenous testosterone production. Testosterone substitution therapy was eventually instituted in 15 patients.
DISCUSSION
A total of 180 past or current AAS users visited the AAS clinic of the Spaarne Gasthuis in Haarlem, the Netherlands, between May 2011 and May 2016. The typical visitor to our clinic is a male, amateur strength athlete, who started using AAS in the second decade of life. Anabolic steroids are mostly used in cycles with a duration between 6 and 18 weeks. The unproven rationale behind this strategy is to gain muscle mass and strength during a cycle, allowing the body to recover between cycles. Since muscle mass and strength start to decline after discontinuation of AAS, multiple cycles or continuous use are deemed necessary to maintain or further increase the gained muscle mass. Some adopt the so-called ‘blast and cruise’ strategy, in which cycles with multiple high dose AAS are alternated with a lower maintenance dose. The contents, dose, and duration of the cycles are mostly directed by advice from self-proclaimed experts and are based on unproven beliefs and personal experience. AAS cycles are rarely identical, which shows that, although most users have strong beliefs about which type, dose and combination of AAS should be optimal for their purpose, there are no widely accepted guidelines. Most AAS cycles contain a type of injectable testosterone ester, generally combined with nandrolone, trenbolone and/or boldenone esters. Our findings are in concordance with questionnaire studies performed among bodybuilders which found similar demographics and comparable characteristics of AAS use.3,8 In addition to AAS, other substances are added, either to increase muscle mass (growth hormone) or to decrease fat mass (clenbuterol, thyroid hormone). Sometimes, medications are used to prevent or treat side effects during or after the cycle: aromatase inhibitors and tamoxifen (against gynecomastia and/or fluid retention), isotretinoin (to treat acne), human chorionic gonadotrophin (against testicular atrophy and/or reduced fertility), sildenafil (to treat erectile dysfunction) or finasteride (to prevent hair loss). As a result of prolonged AAS use, endogenous testosterone production and spermatogenesis are suppressed during and for weeks after the cycle. In an attempt to speed up hormonal recovery as well as to prevent symptoms of androgen withdrawal, most users take post-cycle therapy. PCT mostly consists of a combination of tamoxifen, clomiphene or hCG, usually taken for 2-4 weeks shortly after the end of the cycle with AAS. Although widely used, the efficacy of PCT remains to be determined.
Health risks of AAS abuse
There are several reasons why users of AAS may have an increased risk of health problems. Firstly, most of them fanatically engage in weight training which may lead to symptoms resulting from overburdened muscles, joints and tendons. Secondly, a considerable number of the visitors of our clinic admitted to using drugs, such as XTC, cocaine, cannabis and GHB. The high incidence of recent drug use has been reported previously. Survey studies showed that 23-33% of AAS users meet the criteria for substance dependence disorder compared with 11% of non-AAS users.3,9-11 Most importantly, the use of high-dose androgens and associated substances to treat side effects may have adverse effects. In our 180 patients no critical health issues occurred. The most severe complication was a serious skin infection at the injection site. The large majority of our subjects nevertheless reported one or more side effects related to the use of AAS. The side effects and their frequency of occurrence correlate with those described in earlier studies.8,12,13 Most users were familiar with common side effects such as acne, gynaecomastia, testicular atrophy, fluid retention, agitation and fluctuations in libido and regarded them as inherent to the use of these substances. Most of these side effects were rated by them as mild or temporary and acceptable with respect to the perceived increase in muscle size and strength. A substantial proportion of the reasons for referral to our clinic were related to these side effects, especially when they persisted after discontinuation of the AAS. Side effects that may go undetected by the patient include high blood pressure, abnormal liver biochemistry, polycythaemia, decreased HDL-cholesterol and decreased sperm count. Whereas high blood pressure and polycythaemia were rare findings in our population, lower HDL-cholesterol was frequently encountered. Although low HDL-cholesterol is associated with an increased risk of cardiovascular disease in the general population, it is unclear if and to what magnitude this contributes to cardiovascular morbidity in AAS users, knowing that a decreased HDL-cholesterol may be transient. Mild elevation of aspartate transaminase (ASAT) and alanine transaminase (ALAT) was a common finding in our subjects. Cholestatic liver damage is associated with use of oral AAS, since these compounds are alkylated to prevent extensive metabolism in the liver.14 However, we believe that in most cases, mild elevation of ASAT and ALAT is not a sign of liver damage, but is due to muscle damage associated with extensive strength training. This is also suggested by a clearly elevated level of CK and normal levels of alkaline phosphatase and γ-glutamyltransferase in most subjects. Low sperm count results from suppression of the hypothalamo-pituitary-gonad axis during AAS use. Since supraphysiological doses of AAS are used, suppression of luteinising hormone (LH) and folliclestimulating hormone (FSH) to levels below the limit of detection is inevitable. From male hormonal contraception studies it is known that it may take up to six months after the first injection of testosterone until sperm counts have decreased to 1 million/ml and that the magnitude of suppression may vary between men.15 Both the extent of suppression and time to recovery of spermatogenesis will likely depend on the dose of AAS and cycle length. In our study we only performed semen analysis in the few cases in which reduced fertility was the reason for referral. Moreover, we did not have pre-cycle semen tests. Therefore we were unable to establish a causal relationship between AAS use and impaired semen quality.
Treatment of patients
Persisting side effects despite discontinuation of AAS were the most common reason for referral to the AAS clinic. Mostly, side effects were related to the (perceived) disturbance of male gonadal function, resulting in gynaecomastia, erectile dysfunction, loss of libido and a range of less circumscribed symptoms that may be attributed to low testosterone levels. In most cases reassurance and advice to be patient about spontaneous relief of symptoms was sufficient. Persistent, painful gynaecomastia was treated with tamoxifen 20 mg daily. Although this relieved symptoms in the majority of cases, the chance of recurrence after cessation of therapy appeared to be high. Eventually, many patients chose surgery as a definitive treatment. Post-AAS hypogonadism usually resolved without therapy within six months after the last injection of AAS. Testosterone substitution therapy was reserved for patients with long-term post-AAS hypogonadism who were motivated to stop AAS indefinitely and had a significant symptom burden. It appeared that particularly the subjects with a high cumulative dose of AAS abuse were at increased risk of long-term suppression of endogenous testosterone production. In these cases, endogenous testosterone levels were repeatedly slightly below or above the lower limit for young men and associated with symptoms such as erectile dysfunction, loss of libido, fatigue and depressed mood. A particular drawback of testosterone treatment is that it stops recovery of the function of the hypothalamo-pituitary gonad axis. Especially when adequate spermatogenesis is important, a trial with tamoxifen 20 mg daily may be indicated instead. Tamoxifen acts as an oestrogen antagonist on the hypothalamus and pituitary and stimulates LH and FSH release by the pituitary. In our experience it mildly increases endogenous testosterone production and spermatogenesis. However, in most men the testosterone levels decreased to the pre-treatment levels after stopping tamoxifen. When tamoxifen is not sufficient, hCG 1500 IU twice weekly mostly results in normalisation of endogenous testosterone levels within weeks, followed by restoration of sperm concentration within months.
Limitations of the study
Our study has a few important limitations. Although our clinic is the only clinic dedicated to AAS in the Netherlands, it only provides care for a small minority of the total group of AAS users. It presents a selection of people who were referred or self-referred because of side effects or problematic AAS abuse. Users without health issues would not consult the AAS clinic, therefore the estimated incidence of side effects in our study is probably exaggerated. Similarly, since only users with health problems were selected, their method of use may have been more hazardous. We were unable to verify the concentration and contents of the substances used by our patients. Evaluation, treatment and follow-up of the subjects were not standardised. Patients were either past or current users, and the time between last AAS use and evaluation varied extensively. The current study is retrospective in nature and documentation was incomplete on many items. The documented percentages of types of AAS, PED and medications used as well as side effects reported are likely to be affected by recall bias and reporting bias. Additionally, we were unable to establish a causal relationship between AAS abuse and health issues or abnormal laboratory tests.
Nonetheless, this study is so far the most elaborate to be conducted in the Netherlands. Patients came from all over the country. Our experience with AAS users in the clinic and comparison with literature data have led us to believe that patient characteristics and the mode of AAS use as described in our study is representative for AAS abuse in general. We therefore believe this study gives a good insight into the practice of AAS abuse and its most common side effects and health risks.
Concluding remarks
This review of 180 patients referred to the AAS clinic suggests that AAS abuse does not structurally lead to severe health problems and critical side effects are limited to incidental cases as reported in literature. However, the incidence of side effects with a substantial symptom burden, reduced fertility, substance abuse dependence and potentially harmful concomitant use of other PED and medications among AAS users is high. Considering the large number of users in the community, AAS abuse may be an important public health problem.13 A prospective study with a systematic approach is required to provide more reliable data regarding short- and long-term health risks of AAS abuse. Moreover, we need clinical trials to study the efficacy and long-term effects of treatment.
DISCLOSURES
All authors declare no conflict of interest. No funding or financial support was received.
REFERENCES