

A solitary pulmonary nodule is a frequent incidental finding on routine chest X-rays. The majority of these nodules – especially in the young and non-smoking population – represent a benign (non-cancerous) lesion with a broad differential diagnosis. Since a malignant process is the most important cause to exclude, additional imaging is warranted. In some cases, additional imaging creates a new therapeutic dilemma.
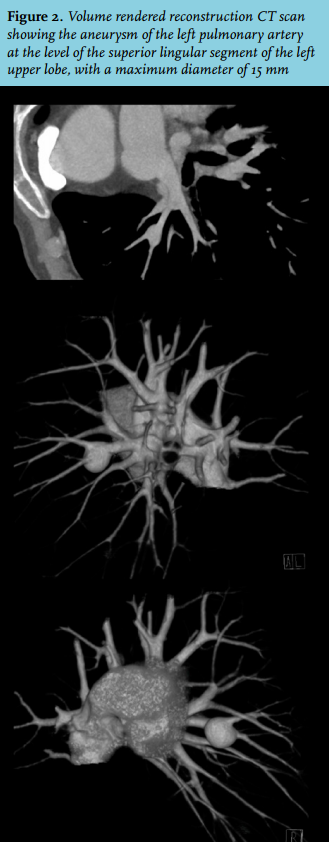
In the present case, computed tomography (CT) scan revealed a bifurcation aneurysm of the left pulmonary artery at the level of the superior lingular segment of the left upper lobe, with a maximum diameter of 15 mm (figure 2). Digital subtraction angiography corroborated these findings, pulmonary artery pressure during this procedure was within normal limits (27/8 mmHg). Patient history, physical and diagnostic examination did not reveal any clues for underlying congenital or acquired conditions that might act as causal mechanism.
The risk to develop a dissection or rupture depends on the actual size of the aneurysm or rate of progression of PAA diameter, and early diagnosis and treatment are crucial for this reason. However, due to the low prevalence of PAA and the diversity of causative factors, no standardised clinical management and treatment guidelines are available. Reported therapeutic options comprise angiographic embolisation or selective exclusion of the aneurysm by means of a covered stent in specific cases, video assisted thoracoscopic (VATS) lobectomy, or active surveillance by means of (annual or bi-annual) CT imaging for smaller aneurysms. Surgical intervention is preferred since it is curative and importantly may also be diagnostic. In order to choose between active surveillance and surgical intervention, there is no clear consensus regarding an adequate cut-off in diameter of the aneurysm, but an aneurysm more than double the size of the normal diameter of the affected vessel has been proposed.
The patient was discussed in a multicentre and multidisciplinary team. Angiographic embolisation of the aneurysm or selective exclusion by means of a covered stent was not possible due to the location at a bifurcation. Therefore, the treatment options comprised active surveillance, selective endovascular occlusion of the afferent vessel with secondary (mild) lung infarction, or VATS lobectomy. After weighing the advantages and disadvantages of the various therapies and in compliance with the fact that patient was reluctant to undergo surgery, we mutually agreed to opt for an active surveillance approach with regular reassessment of aneurysm diameter. CT imaging at six months did not show any change in aneurysm size and patient was still free of symptoms with an unaltered chest X-ray at 12 months of follow-up. He will undergo periodic reviews in the future.
DISCLOSURES
The authors declare no conflicts of interest.
REFERENCES