

KEYWORDS
Caregiver, emergency department, geriatrics, preventability
INTRODUCTION
Background
Our population is ageing, and older people represent an increasing proportion of patients who visit the emergency department (ED).1-5 In the Netherlands, ED visits by older patients are also increasing. This may be associated with recent changes in Dutch healthcare such as the reduction of nursing home beds, resulting in (potentially vulnerable) older people living independently at home for a longer period of time.6
Older patients frequently suffer from multiple conditions,7-9 often accompanied by polypharmacy.7 In addition, older ED patients generally have atypical clinical presentations, more serious illnesses, higher diagnostic test use, and require more staff time and overall resources when compared with younger patients. Consequently, older age is associated with a longer ED length of stay (LOS) and a higher admission rate, both of which contribute to ED crowding.1-4 ED crowding is in turn, linked to prolonged ED LOS, reduced quality of care, impaired access, and an increased risk of adverse events. In addition, crowding is a financial burden for both patients and healthcare institutions.10,11
An ED visit can also have a profound impact on patients themselves; for example, more than one in three older patients experience an adverse outcome within 90 days of ED discharge.12 Furthermore, ED admissions often lead to a decline in independency.13,14
Preventing certain ED visits—when possible—with active and personalised interventions in the acute care chain may be more patient-friendly and cost-effective than usual care. To achieve this, it is important to identify contributing factors that lead to ‘preventable’ ED visits. Unfortunately, there is no generally recognised definition of preventable ED visits. This could in part, be explained by the fact that perspectives on preventability are system-dependent and rely on how acute care is organised. Consequently, viewpoints are expected to be different between countries. Real-time perspectives of patient and healthcare workers on preventability of ED visits may provide important insights.15-17 Therefore, we performed this prospective, observational study on the preventability of 200 ED visits by patients aged 70 years and older in a Dutch teaching hospital.
The objective of this study was to evaluate the opinions of patients, their caregivers, ED physicians (EPs), and general practitioners (GPs) on the preventability of an ED visit.
MATERIALS AND METHODS
Study design and setting
In the Netherlands, primary healthcare is well developed and accessible for patients 24 hrs a day. General practitioners (GPs) serve as gatekeepers to hospital care. During office hours, patients can consult their own GP, usually obtaining an appointment that day. After-hours primary care is provided through GP cooperatives.10 The majority of ED patients are referred by their GP or by ambulance. Self-referrals compromise a small minority.11 This prospective, mixed-method observational and qualitative study took place in a regional teaching hospital in the Netherlands with a yearly ED attendance of 25,000 patients in 2017; 31% of patients were ≥ 70 years of age. Data collection took place between July 24th and September 7th, 2017. The study was approved by the institutional Ethics Committee of VieCuri Medical Centre, Venlo, the Netherlands.
Patients
All patients ≥ 70 years of age who visited the ED in the study period were eligible for inclusion. Trauma-related ED visits were excluded except for visits involving a fall, because it was assumed that older people who, for example, suffer from a traffic accident, are less vulnerable. Patients were also excluded if they were not able to give written informed consent and if no legal representative was present, or if a language barrier was present. All patients gave written consent prior to the interview. Patients were included only during the time the site researcher (MV) was present. To reduce selection bias, MV worked in five random eight-hour shifts per week, both during office hours and after hours, including weekend days.
Sample size justification
To our knowledge, this was the first study to investigate the perspectives of patients and their caregivers on their ED visit, so it was not possible to conduct a power analysis. Therefore, inclusion was stopped after reaching 200 cases, which is similar to comparable studies on patient perspectives on preventability of readmissions.15-17 Moreover, the sample size and sampling method (true random sampling) we used were shown to be the best method in a study which compared four sampling methods for observational studies in the ED. It represented the overall population for more than 95% of the samples and the probability of selection bias was low.18
The primary outcome was defined as if the patient, caregiver, GP, and EP considered an ED visit preventable or not. Secondary outcomes were consensus of preventability and the qualitative data derived from the interviews. Our hypothesis was that professionals would consider an ED visit preventable more often than patients and their caregivers.
Data collection
Data were collected from semi-structured interviews with the patients, their caregivers, and GPs by MV, the first author of this manuscript. The interviews were tested in a pilot patient group before we agreed on a final version. MV is a female medical master student (BSc) with two years of clinical experience. During the study period, MV was not directly involved in patient care. Interviews took place in each patient’s room and lasted approximately 30 minutes (duration was not recorded). Patients and caregivers (defined as a person providing unpaid intensive and long-term care because of a personal relationship) were not separated during the interview. Before the interview commenced, participants were informed that the researcher aimed to assess their opinions about the ED visit, but they were not informed about the hypothesis of the study group. Subsequently, patients and providers were asked about the reason for the ED visit and whether they thought the ED visit could have been prevented, which was questioned in the following way: “Do you feel the current ED visit was preventable in any manner, by anyone?”. Possible options were “yes”, “no”, or “unknown”. All interviewees were asked which event(s) had led to the ED visit and what could have been done to prevent this visit. It was possible to appoint more than one event. In addition, the vulnerability of the patient was determined by a combination of questions (see Appendix A for the questionnaire). During the interview, field notes were recorded by the interviewer. No repeat interviews took place. EPs (who were the physicians caring for the patient in the ED and included both board-certified EPs and junior physicians in different specialties) were provided with written surveys. A semi-structured interview was held with the GP by telephone. If the patient’s personal GP was not available, the locum GP was consulted. Subsequently, the answers were clustered into categories (open coding followed by axial coding; see Appendix B) by MV and an EP (author DB). In cases of disagreement, an internist (author FS) was consulted. No feedback was provided to participants on the findings.
Apart from the interviews, a structured medical record review was performed in which information was collected regarding vulnerability, comorbidity, and medication. We defined polypharmacy as the concomitant use of five or more drugs.19 Different scores (such as the Charlson Comorbidity Index [CACI]20 and the Acutely Presenting Older Patient [APOP] score)21 were calculated, combining information from the interviews and the medical record. Office hours were defined as weekdays between 08.00 hrs and 16.59 hrs. Out-of-office hours were weekdays between 17.00 hrs and 07.59 hrs and during the weekend.
Statistical analysis
Baseline characteristics were presented as the number and percentage for categorical variables and as mean and standard deviation (SD) for continuous variables (in case of a non-normal distribution, we presented median [range]). For analysis of preventability in subgroups (triage category, way of referral, cognitive decline, etc.), we used the Pearson’s chi-square and Fisher’s exact test for dichotomous and categorical data. The Mann-Whitney U test was used for continuous variables. Differences were considered statistically significant at a p -value of less than 0.05. Cohen’s kappa (κ) was used to measure agreement of preventability assessments (options “yes”, “no”, and “unknown”) separately for each pair of four interviewed groups. We defined kappa values between 0.00 and 0.20 as slight agreement, between 0.21 and 0.40 as fair agreement, between 0.41 and 0.60 as moderate agreement, between 0.61 and 0.80 as substantial agreement, and between 0.81 and 1.00 as almost perfect or perfect agreement.22 Statistical analysis was performed in IBM Statistics SPSS V.22.0.
RESULTS
Patient characteristics
During the study period, 372 eligible patients aged ≥ 70 years visited the ED during the time MV was present, of whom 200 were included (inclusion rate of 53.8%).
The reasons for exclusion (n = 172) were trauma-related (n = 81; 47%), participation refusal (n = 31; 18%), no possibility of obtaining informed consent (n = 31; 18%), language barrier (n = 19; 11%), and other (i.e., too ill or nonresponsive; n = 10; 6%). In the study period, 456 eligible patients were missed because the site researcher (SR) was not present. The median age of participants was 79.0 years (range 73-85 years), 50.5% were female, and 79% presented during office hours. Most (95%) lived independently before the ED visit. Twenty-three percent of patients reported domiciliary care, 21.5% a caregiver, and 29.5% both. A large proportion (69.5%) used five or more drugs at the time of the ED visit. The mean CACI score was 5.4 (SD: 1.96), and the median risks of functional decline and mortality according to the APOP score were 28.0% (range 16-45) and 7.0% (range 3-14), respectively. Patient characteristics are summarised in table 1. 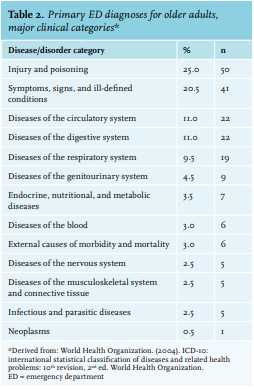
Preventability
Patients regarded 12.2% of ED visits preventable, caregivers 9%, GPs 20.7%, and EPs 31.2%. The assessment per interviewed group is listed in table 3. EPs were more likely to consider visits preventable during office hours than during after-hours (34.4% [54 of 157] vs 19.0% [8 of 42]; p = 0.001). The experience of the EPs was also relevant to their judgment: board-certified EPs considered the visits preventable significantly more often than did junior doctors (45.8% vs 26.5%; p = 0.033). Subgroup analyses for triage category, referral by a locum GP, polypharmacy, APOP score, CACI score, cognitive decline, living situation, and medical specialty showed no significant differences. Also, no difference was found between patients who were admitted and discharged from the ED.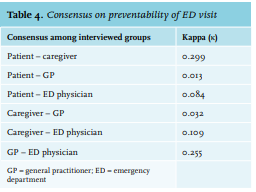
Table 4 shows Cohen’s kappa for the consensus on the opinions among the interviewed groups. None of the kappas were satisfactory; they were all below κ = 0.3. The poorest agreement was found between patient and GP and between caregiver and GP, with κ = 0.013 and κ = 0.032, respectively. The highest kappa was found for patient and caregiver and for GP and EP, with a rate of κ = 0.299 and κ = 0.255, respectively.
Patients’ and providers’ perceptions
Qualitative data derived from interviews with patients, caregivers, GPs, and EPs revealed different perspectives between the groups. Participants who answered “yes” or “unknown” on the question about the preventability of an ED visit were included in this analysis. For all interviewees, it was possible to sum up multiple causes. The patients who answered “yes” or “don’t know” (n = 65) most frequently blamed themselves for the visit, saying they should have called for help earlier or should have been more careful to prevent themselves from falling (17/65). Other frequently mentioned causes by patients were related to hospital care (i.e., early discharge and better follow-up [13/65]) or primary care (i.e., fall prevention, other/earlier intervention [10/65]). Caregivers (n = 37) frequently mentioned that the ED visit could have been prevented if the GP had acted earlier (10/37), if hospital doctors had communicated better with the patient during an earlier admission (6/37), or if they had not discharged the patient too early (5/37). GPs (n = 65) often wanted to refer a patient to a specialist but could not obtain an appointment that met their expectations in terms of timeframe, thus ultimately sending the patient to the ED (19/65). Also, GPs mentioned patient-related factors, such as avoiding care (9/65) or calling the ambulance instead of the GP (5/65). EPs (n = 72) most often mentioned aspects of GP care as a contributing factor, stating that the GP could have visited the patient earlier (5/72), could have treated the patient him/herself (9/72), or would not have referred the patient to the ED after a more thorough discussion with the patient and his/her family (4/72). EPs thought better communication between GPs and specialists could have prevented some visits as well (12/72).
DISCUSSION
The purpose of this present study was to assess the opinions of the patient, caregiver, GP, and EP on the preventability of an ED visit. Patients considered 12.2% of their ED visits preventable. Caregivers, GPs, and EPs regarded ED visits as preventable (9.0%, 20.7%, and 31.2%, respectively). Patients and caregivers, and GPs and EPs had the highest consensus, but their kappa measurements were still very poor. Although patients most frequently blamed themselves, healthcare providers predominantly mentioned lack of communication and organisational issues as contributing factors to preventable ED visits in older patients.
ED patient profiles
To our knowledge, this is the first study to assess the preventability of ED visits by using perspectives of patients and their providers. However, it is not the first study to define the older population in the ED. Median age, gender distribution, and reasons for ED visits are comparable with previous studies.5,21,23 In our cohort, 24% of ED visits were fall-related, and almost half of our patients (49.5%) experienced a fall in the six months prior to their visit, which confirms findings of previous studies.1,2,24 In addition, the polypharmacy rate was in agreement with earlier studies in older ED patients.1,7 Both the mean CACI score of 5.4 (which means the estimated relative mortality risk in our group was higher than 6.38% [CI: 3.07-13.2]) and the high median risks of functional decline and of mortality measured by the APOP score show the high degree of vulnerability in our study population.20,21 Despite being vulnerable, almost all patients lived independently (95%).
Preventability
Nearly all previous studies on patients’ perspectives on preventability assessed readmissions.15,16,25,26 One study did investigate the preventability of ED visits, but that study’s objective was to understand the patient’s perspective on the circumstances that led to the ED visit, not the preventability of the visit. It did not include all stakeholders and questioned patients retrospectively.27 A recent British study estimated that 19.4% of ED attendances could be avoided, based on a survey filled in by senior consultants within the ED. According to their analysis, ED visits of patients older than 65 years (5%) were less likely to be deemed avoidable than those in patients younger than 16 years (34.9%) or adults aged 16 to 64 years (18.5%). However, the researchers’ method of determining this was completely different from that in our study. We also believe that some of the items in the checklist used to define appropriate ED visits are not exclusively linked to appropriateness, such as arrival by ambulance or overnight stay in a facility. Older people are sometimes admitted for nonmedical reasons, which does not directly mean the ED visit was appropriate.28
In our study, EPs considered 31.2% of ED visits preventable, which means they believed that these patients could have been managed effectively by other health service providers. If one in three ED visits by older patients can be diverted or prevented, this would benefit both patients and EDs. The high percentage of preventability attributed by EPs is probably due to their knowledge about alternatives to hospital care. This hypothesis is strengthened by the fact that EPs were more likely to consider ED visits preventable during office hours than during after-hours (34.4% vs 19.0%). However, hindsight bias might have played a role in the EPs’ judgment of preventability: in cases of negative diagnostic testing, the post-test probability of regarding an ED visit preventable is much higher than the pre-test probability (which is applicable to GPs). This may be the reason why GPs considered ED visits less-often preventable than their hospital colleagues, even though some of the GPs also knew the ED visit outcome when they were interviewed. Only 1:8 patients and 1:10 caregivers thought their visit was preventable. Poor consensus was found among the different groups. Patients and caregivers agreed most often, probably because of their similar perspectives. The same applies to the perspectives of GPs and EPs, who likely have similar professional views. Little agreement was found between patients and GPs and in particular, between caregivers and GPs. This confirms previous studies on the preventability of readmissions, which also show little consensus among patients and professionals.25 Ideally, patients and providers speak the same language, resulting in better agreement between patients and providers toward their expectations of emergency care. It would be interesting to investigate whether better communication and/or shared decision making improves consensus and lowers utilisation of emergency care services.
Limitations
This study has several limitations. First, the SR was not present 24 hours per day. To reduce selection bias, the SR was scheduled in random shifts. This ‘true random sampling’ method has been shown to represent the overall population for more than 95% of the samples and it has a low probability of selection bias.18 To assess generalisability, we compared our study population with all eligible patients who visited the ED in the same study period. Almost all patient characteristics were comparable, except for the presenting time; the study’s patients presented more frequently during office hours (79.0% vs 31.7%). Only few previous studies described the time of ED presentation and showed that most older people presented during weekdays (71.9%),5 especially in the morning and late afternoon.2 Second, education level and possible cognitive impairment were not measured systematically. These could have been influencing factors in the selection of participants. Third, the number of respondents varied between groups, with the smallest numbers in the caregiver and GP group. Half of the patients did not have a caregiver, and 13% of the GPs refused to participate in the study. Fourth, this was a single-site study, which reduces the generalisability of our findings to other hospitals or countries. Fifth, we included only Dutch-speaking patients, which could be a limitation because of the increasing multicultural aspect of our society. Sixth, trauma-related visits (except for those involving a fall) were excluded as it was assumed that these patients are generally less vulnerable. The exclusion of non-fall related injuries may have caused some bias as not all older patients who, for example, drive a car are fit, and some accidents might have been preventable. This would be an interesting topic for future research. In addition, for the qualitative part of the study, we did not assess whether saturation was reached. However, because of the extensive sample size of 200 patients the probability of data saturation is high. During the interview, no audio or visual recording was used to collect data. Instead, the input was collected by field notes and subsequently categorised. The results of the qualitative part of our study should therefore be interpreted with caution. Finally, patients and caregivers were not separated during the interview and could have influenced each other’s answers. However, the low kappa measurement shows great nonconformity between the groups.
To be improve upon our findings, future studies should be multi-centre, with a better balance of patients who present during office hours and after hours. There should also be more focus on the reasons for the disparity between the perspectives of all stakeholders, which, for example, can be assessed through focus group research. Finally, it should be investigated whether better communication and/ or shared decision making improves consensus among patients and providers and subsequently lowers ED visits.
CONCLUSIONS
In this study, patients and caregivers consider an ED visit preventable less frequently than professionals, who consider a visit preventable in almost one-third of all visits. Little consensus is found among professionals and patients or their caregivers, and all groups have different perspectives on the contributing factors of a preventable visit. To our knowledge, this is the first study to provide insight into the preventability of ED visits in the elderly according to patients, their caregivers, GPs, and EPs. To help improve geriatric ED care, future studies should focus on the differences between the opinions of patients and providers and how to align those involved in care.
ACKNOWLEDGMENTS
We would like to thank all patients, caregivers, GPs, and EPs for their participation in the study. We are also grateful for the support of the GP cooperative Cohesie.
REFERENCES
APPENDIX A:
APPENDIX B