

INTRODUCTION
Vasospastic angina (VA), also known as Prinzmetal angina, is a less common form of angina in which spams of the coronary arteries cause typical anginal symptoms along with ST-segment deviation. Long lasting VA may result in myocardial ischaemia, potentially leading to life-threatening ventricular arrhythmias. Calcium channel blockers (CCBs) and nitrates are the most frequently used drugs that may, in high dosages, provide symptom relieve in 30-80% of these patients.1 In order to further improve symptom relief, novel invasive treatment options such as renal denervation (RDN) are currently being studied.2,3 Here, we present a case with refractory VA undergoing RDN. It is our aim to create awareness for the potential lethal consequences of inadvertent changes in chronic medical treatment in vulnerable patients with VA.
CASE DESCRIPTION
A 46-year-old woman with refractory VA with confirmed spasm of the right coronary artery (RCA) and recurrent ventricular tachycardia leading to implantable cardioverter defibrillator (ICD) shocks, was referred to undergo renal denervation (RDN). In order to control the VA episodes, she used verapamil with controlled release (CR) (total daily dose (TDD) 480 mg), isosorbide mononitrate CR (TDD 120 mg), and perindopril (TDD 2 mg). 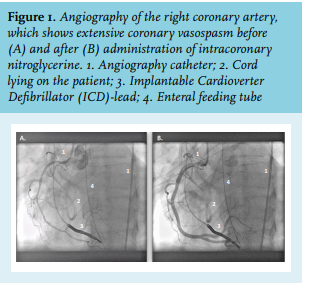
DISCUSSION
The differential diagnosis of this unexpected cardiac arrest included CCB poisoning due to the clinical presentation of severe cardiogenic shock. However, when critically reviewing her medication charts, it became clear that from the moment she arrived at the hospital up until the first cardiac arrest, that the patient had received only one dose of direct release CCB in a dose of 120 mg in the morning; the afternoon dose was not given, probably because the patient was away for the procedure and somnolent afterwards. CCB poisoning was therefore not plausible. An association with the RDN was considered, but in light of the pathophysiological mechanism, this seemed unlikely.2
However, the abrupt switch of high-dose verapamil with controlled release (240 mg twice daily) to direct release 120 mg, which she received only once, could lead to the so-called CCB withdrawal phenomenon (figure 2).4 This phenomenon is characterised by clinical symptoms similar to CCB poisoning, including nausea, vomiting, and cardiogenic shock. The mechanism behind this CCB withdrawal phenomenon is largely unknown, but a commonly adapted theory is that CCB use results in a depletion of calcium in the smooth muscle cells (SMCs).5-7 Because of this, the calcium gradient between extracellular and intracellular calcium of SMCs is high and calcium will follow this gradient towards the inside of the SMCs. Upon abrupt withdrawal of CCBs, a burst of calcium will enter the cell and cause depolarisation of the cell wall, resulting in prolonged contraction of the SMC and ultimately lead to coronary vasospasm. Patients with VA are more prone to experiencing vasospasm by CCB withdrawal.8-10 Experimental evidence would further elucidate the pathophysiology of this phenomenon. In addition, it is known that low-dose nitrates, which cause venous vasodilation, are insufficient to prevent coronary spams due to the required arterial vasodilation. Termination early after the procedure, as could have been the case, would certainly have contributed to the course of events. Independent of the exact stop of nitroglycerine, so before or after the event, the patient’s records show that both the CCB as nitrate therapy were sub-therapeutic at the time of cardiac arrest (figure 2).4
CONCLUSION
This case demonstrates that acute withdrawal of CCBs can have severe consequences, especially in patients with VA, who can be considered high-risk patients. This can result from drug substitutions, which are sometimes inevitable, for example, due to local limited availability of drugs, and in this case, drug substitution led to inadequate therapy of critical medication for a patient with VA. In addition, treatment of this syndrome is difficult, as an arterial spasm is always confirmed after the occurrence of symptoms. ECMO therapy, while lifesaving, may not be available in most hospitals, which means that prevention of CCB withdrawal syndrome is essential. This case highlights the need to carefully monitor the process of drug substitution with respect to equal therapeutic dosages to prevent unintentional changes in essential medication.
DISCLOSURES
Joost Daemen has received institutional research support from Medtronic, Acist Medical, Abbott, Pie Medical, and PulseCath, and received consultancy fees from PulseCath, Acist Medical, and Medtronic, although not for this particular article. Other authors declare no conflicts of interest.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
REFERENCES